Healthcare funding in South Africa – medical aid schemes coverage versus universal coverage
Medical aids have been in the crossfire since the NHI Bill was signed into law by President Cyril Ramaphosa in May 2024. Even without this threat, medical aids are, according to the Who Owns Whom report on medical aid funding in South Africa [found here], coming under growing strain due to the increasingly high costs of private healthcare.
It is worth looking into what is driving ever-increasing healthcare costs and the sobering view on the NHI.
Population coverage and revenue base
South Africa’s private sector medical aid industry is regarded as unsustainable as it stands, as it serves only about 15% of the population, hence the aspiration for universal coverage through the NHI. Private sector healthcare competes with the best in the world in terms of quality and efficiency of service, but it is very expensive.
In a stagnant economy with income per capita regressing, it comes as no surprise that medical aids, especially the open schemes, are seeing a decline in membership and a shift toward cheaper options in their product line-up.
The inclusion of prescribed minimum benefits (PMBs), the 25% minimum statutory solvency cushion and continued above-inflation cost increases have pushed up the average cost of medical aid premiums substantially.
Cost drivers of medical aid premiums
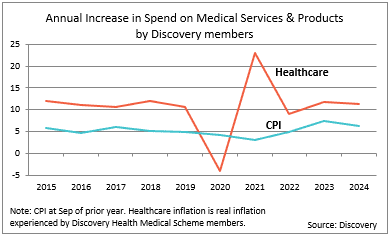
The cost increases are attributed to several causes such as the price pressure of medical services delivery, partly due to innovation with newer and better solutions, and the higher usage of medical services by ageing members who can still afford the high cost of medical aid cover.
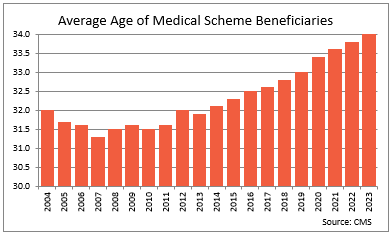
The ageing membership is a result of younger households with lower salaries not being able to afford the high cost of membership, and because people with medical cover live a healthier lifestyle and therefore have a longer life expectancy. A feature of medical insurance is that the balance is maintained by healthy members subsidising unhealthy ones. An ageing membership tips this balance.
Healthcare cover options and disadvantages
These issues have created a big gap in the market which has been filled with some lower cost health insurance products that exclude minimum prescribed minimum benefits. These products do not cover major illnesses such as cancer, the treatment of which has become exceptionally expensive. For example, one advanced PET scan can cost over R50,000 and these kinds of numbers are often only a fraction of the full cost of surgical intervention and treatment, even for medical aid members, as disbursement limitations and co-payments are all too common.
Why the NHI, and is it feasible?
In principle, the government has a compelling case to introduce NHI, although the way it is conceptualised, and the proposed implementation plan, are swamped with hurdles and concerns. Most more developed countries have some form of universal healthcare, but some also struggle to fund the sector. South Africa faces two major challenges – that it does not have the financial means to support the universal healthcare system it is proposing, and, perhaps more importantly, that there is a fundamental distrust about government’s capacity to run an NHI without it going the same way as almost all parastatals that have gone to complete ruin.
Important facts about transitioning to NHI
Some statistics reveal the momentous task of transitioning to a universal health system. Currently government spends about R272bn on 85% of the population (or about 55 million people), amounting to R4,945 per person per year. Private medical aid contributions amount to approximately R260bn for an estimated 10 million beneficiaries or R26,000 per person. If a universal system is introduced then total spend of R532bn for 65 million people would equate to R8,184 per person. Supposing that private sector members’ contributions are maintained, the average available to them would drop from R26,000 to R8,184. The contention is that private sector medical providers’ cost structures cannot be reduced by such an amount to provide the same level of service. The 15% of the population on medical aid do not have the means to fund the shortfall, nor does the government have the funds to increase its health budget by about R1.1tn.
Ideal way forward
A more effective long-term transition model is needed, one that would largely maintain private sector participation and incentives while crafting a feasible roadmap toward universal access to quality health care and a thriving industry.
Contact us to access WOW's quality research on African industries and business
Contact UsRelated Articles
BlogCountries Human health and social work activitiesSouth Africa
South Africa’s Healthcare Challenges and the Future of Universal Health Coverage
Contents [hide] Healthcare is a vital cog in any economy. When the nation’s workforce is healthy, there is more economic activity, businesses do well with less absenteeism and highly productive...
BlogCountries Human health and social work activitiesSouth Africa
The cleaning products industry – trends and sustainability
Learn about South Africa's cleaning products: sustainability trends, brand dynamics, SME opportunities, growth outlook, exports & eco-packaging shifts.
BlogCountries Human health and social work activitiesSouth Africa
Is the South African healthcare sector in crisis?
Contents [hide] Introduction Information on the healthcare sector is plentiful and summarised in the latest WOW report on the healthcare sector in South Africa. Besides the issue of the relatively...